This is a carousel. Use Next and Previous buttons to navigate
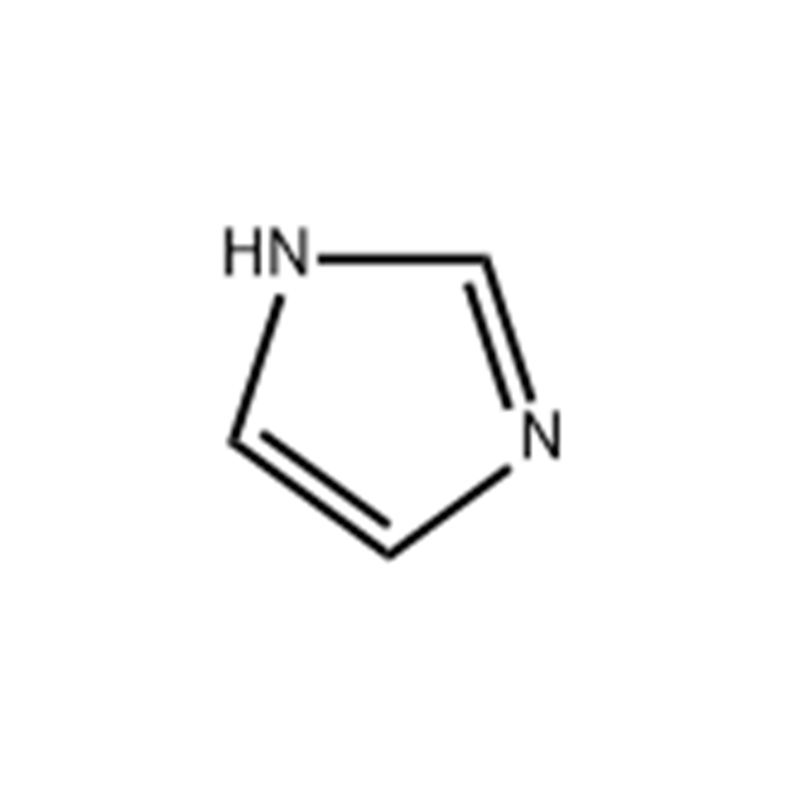
Breast cancer survivor Judy Howell, 70, has a check-in visit with her doctor C. Kent Osborne who is the founding director of the Dan L. Duncan Comprehensive Cancer Center at Baylor College of Medicine, Wednesday, Nov. 2, 2022, in Houston. Howell had a DIEP flap procedure in which tissue from the belly was taken to reconstruct the breast after getting a double mastectomy. Amidinosarcosine Monohydrate
Judy Howell stared up at her ultrasound technician and asked, “I’ve got breast cancer, don’t I?”
The Montrose resident was not surprised when the answer was yes.
“I had 30 years to mentally prepare for it,” she said. “I knew one day I was probably going to get it.”
Her sister, Patricia Wakefield, died of breast cancer at age 36. She had found a small lump only a few years earlier.
“It was so tiny that the mammogram was inconclusive,” Howell said. “Eight months later, it grew to the size of a navel orange, and by that time, it had spread.”
Howell stood by her sister’s side through the chemotherapy, radiation and surgery. None of the treatments slowed the cancer’s progression.
Howell, 70, has worried about breast cancer ever since. She started getting her mammogram early, at age 31, and her appointments were scheduled regularly.
That is, until November 2018, when she had to put off her routine mammogram and ultrasound for a number of reasons. Around the same time, she noticed a pain in her breast but assumed it was only a cyst. She had experienced them before, and they were always benign.
In February 2019, Howell finally checked in for her mammogram and received the news. Because she had been thinking about it for so long, she didn’t hesitate to move forward with her treatment.
She knew where she wanted to go, Baylor College of Medicine. She had previously worked at the institution as senior director of development and was involved with building community relations. In fact, she had worked on the campaign that led to the creation of the Lester and Sue Smith Breast Center, part of the Dan L Duncan Comprehensive Cancer Center at Baylor St. Luke’s Medical Center.
Now, she would go there as a patient.
In March 2019, Howell’s biopsy revealed that she had triple-negative matrix-producing metaplastic breast cancer.
Her breast oncologist, Dr. C. Kent Osborne, professor and founding director of the Dan L Duncan Comprehensive Cancer Center, explained that the term “triple negative” refers to breast cancers that test negative for estrogen and progesterone receptors, as well as excess HER2 protein. These cancers tend to grow and spread faster and usually have limited treatment options, other than chemotherapy.
“Matrix-producing metaplastic” is also a rare — and aggressive — subtype. Howell had every reason to expect the same difficulties that she had seen her sister face.
“My sister was so sick, in and out of the hospital,” Howell recalled. “Those three years were misery. I was expecting that.”
Howell soon learned, however, that a lot has changed over time.
Osborne has witnessed that evolution firsthand. “I’ve been doing this for 50 years,” he said.
When he was interning in 1972, all breast cancer patients were treated basically the same — with a radical mastectomy, removing the entire breast, underarm lymph nodes and muscles in the chest wall.
“Most tumors were fairly large by the time they were discovered,” Osborne said. Widespread clinical use of mammograms was still fairly new.
“Chemotherapy was also very primitive then,” he said. “And endocrine therapy to block estrogen in patients was even more primitive.”
Surgeons would also remove the patient’s pituitary and adrenal glands, as well as the ovaries, Osborne said, in an effort to block estrogen from causing the tumor to grow.
“Then things really started to change,” he said. “Breast cancer was recognized as a systemic disease.”
It was no longer simply about the tumor in the breast and adjacent lymph nodes — but also about the microscopic seeds of the tumor that could have spread to other organs.
Removing the breast, lymph nodes under the arm and chest muscles would not improve the patient’s survival rates if the cancer had metastasized to other organs.
This meant that a lumpectomy was a viable option, coupled with radiation. It also suggested that, in addition, a systemic therapy was needed to kill the metastatic seeds, Osborne explained.
The next important advancement was discovering hormone receptor-positive breast cancer cells, with estrogen or progesterone receptors, or both.
The estrogen receptor was identified in the late 1960s, but its application to breast cancer did not occur until a decade later. Only tumors with the estrogen receptor were being driven by the hormone and would benefit from therapies that could block it, he said.
Osborne was a postdoctoral fellow at this point and was involved in several publications on the topic. “We started doing endocrine therapy only for estrogen receptor-positive cancers,” he said. “About 70 percent of breast cancers are now recognized as hormone receptor-positive.”
In the 1980s, more effective chemotherapy developed — by combining the drugs used. Osborne said the years of intense study of the biology of breast cancer led to better treatment options in the 1990s.
For instance, the discovery of the protein called human epidermal growth factor receptor 2 (HER2) led to the development of multiple therapies to block HER2. Some patients with this HER2-positive breast cancer do not need chemotherapy at all — only the drugs that block the protein. Research is ongoing to identify which patients would benefit from which treatment, Osborne said.
Until recently, triple-negative breast cancer has been the least impacted by advances. “But progress through research is starting to change things,” Osborne said. “We’re learning a lot more about triple-negative disease. I think the next big discovery will be in this type.”
Already, doctors are finding antibody treatments and immunotherapies to help triple-negative patients.
“Now we are in the era of precision medicine,” Osborne said. “And it’s an exciting time. Breast cancer is really a group of diseases — not just one at all.”
No two cancers are exactly alike, he said. The various gene mutations that cause the cancer to form and grow are examined.
“It’s like a tumor fingerprint,” Osborne said. “I think that eventually we will have separate treatments for each individual patient — including those with triple-negative breast cancer.”
Howell has benefited from these scientific advancements in treatment
First, she started with multiple chemotherapy drugs before her surgery. In April, she underwent a two-month regimen of adriamycin and cyclophosphamide. In May, she began Taxol for another four courses.
Howell also took medications to counter the side effects of chemo.
Osborne explained that, in the past, chemotherapy would lower white blood cell counts that fight infection, which could cause patients to end up back in the hospital for strong antibiotics.
“That side effect has essentially gone away,” he said.
Howell was prescribed Neulasta, which stimulates white cell production, and medications to prevent allergic reactions and nausea. She did not experience any nausea, but fatigue was an issue. In fact, she was able to continue working during chemotherapy.
Howell also received Xeloda, a drug that came to the U.S. in 2001 and blocks residual cancer cells that remain in the breast after chemotherapy. These cells are discovered during surgery.
Since her treatment, things already have changed, Osborne said. She would have received immunology in addition to chemotherapy instead of the medication if she were to go in today.
“Progress is moving at a faster pace for this less-common type of breast cancer,” Osborne said.
Howell did not undergo radiation, but her surgical oncologist, Dr. Alastair Thompson explained that radiation has changed, too.
“Modern radiation is incredibly sophisticated and very targeted,” he said, comparing the old methods to a push-button phone. “Now we have Samsungs and iPhone 14s,” he said. “It has evolved enormously and continues to improve.”
Surgery has also become more refined, giving patients more options.
“The thing I love about these doctors is they don’t tell you what to do, they ask you what you want,” Howell said.
Thompson, professor and section chief of breast surgery at Baylor College of Medicine, said his goal is to ensure patients are well-informed and have time to talk with their loved ones.
“The first time I meet people, I don’t get to a point where they have to make a decision,” he said. Instead, he goes over the options, mastectomy or lumpectomy, then gives them time to think and discuss.
“It’s a patient’s choice,” Thompson said.“It’s very rewarding to guide people through this and make it a little bump in the road rather than hitting a brick wall.”
These days, lumpectomies are more sophisticated — and actually use magnetic seeds to precisely locate the tumor.
Howell opted for a double mastectomy — and even that has drastically evolved, Thompson said.
“There’s the mastectomy most people imagine — the radical mastectomy,” Thompson said. “And that’s the way mastectomy once was. Nowadays, we leave most of the skin, like an envelope, which can be filled by a plastic surgeon.”
There are options to spare the skin — and sometimes the nipple, depending on the patient. Thompson said that skin-sparing mastectomies have become available only in the past 10 to 15 years, and at Baylor, it is now the standard approach.
“These are not simple things to do,” Thompson said. “It’s a bit of a journey. Having the expertise of a plastic surgeon is key. We can get rid of the cancer and, at the same time, begin rebuilding. It can be very effective.”
When Howell expressed interest in reconstruction, Thompson referred her to Dr. Marco Maricevich, associate professor of plastic surgery at Baylor College of Medicine.
“He got me in to see him that same day, within the hour,” Howell said. The surgical team works closely together and shares expertise.
“What we’re trying to do is piece together all the team players a person needs,” Thompson said. “The patient is at the center.”
Reconstruction can now begin during the mastectomy. Patients talk to both the surgical oncologist and plastic surgeon at the same time, instead of separately.
“Treatment also entails reconstruction,” Maricevich said. “Most patients are really upset and sad with the diagnosis. Our goal is to lift them up and show them all the possibilities — which are many.”
The two main choices are implant-based or tissue-based, also called DIEP flap, which stands for deep inferior epigastric perforators. “We now have the ability to use the patient’s own tissue to reconstruct the breast,” Maricevich said.
The most common donor site is the abdominal wall, without disturbing the muscles. Tissue can also be taken from the thigh, back or buttocks. Blood vessels are taken from the donation site and reconnected to the breast.
Further advances are in the works to reconnect a nerve, as well, to the chest wall. “That is the next frontier in breast reconstruction,” Maricevich said.
The procedure can now be performed through microsurgery, which leaves almost no scarring.
“We try to hide the scar as much as possible,” Maricevich said. “We want to restore the self-esteem of the patients. My patients will be confident, and they can put the cancer behind them.”
He said that in the past, patients would feel disfigured, like they had an amputation. He is working hard to ensure those days are gone.
“We are part of a journey of hope,” he said. “And at the end, most patients don’t have to think about the cancer. They are survivors. They feel good and look good. That’s the main goal.”
Howell’s double mastectomy was performed Aug. 1, 2019. While still under anesthesia, Maricevich began the microsurgery DIEP flap procedure.
After recovery, Howell removed her bandages.
“I was so shocked and surprised,” she recalled. “I thought, ‘Where are the scars?’ I was just astonished.”
Because her nipple had to be removed, Maricevich explained, the entire operation was performed through a small incision in the area. Then, at a later surgery in May 2020, he reconstructed a nipple, and an areola was tattooed.
“The scar was completely masked by the ink of the tattoo,” Maricevich said. “While every case is different, we try to conceal as much as we can. Patients do not have any evidence — or stigma. In the end, it’s all about restoring the quality of life — and getting the cancer completely behind them.”
And that is exactly how Howell feels, she said.
“The type of gratitude I have, I just can't explain the depths of it,” she said. “They’re a dream team. They played such a huge role in shepherding me back into feeling not like a walking cancer patient, but a normal person again.”
Howell continues to visit Osborne every six months for a checkup — and is in two different online support groups. She often recommends others to Baylor and has developed a tip sheet to share with patients.
Early detection is key, she said. Then, she suggests finding the best doctors available.
“It’s important to find the most qualified surgeons who do this day in and day out, who keep up with advances in treatment,” Howell said. “Your life can depend on getting the right doctors. And being in Houston, there’s no excuse for not getting the best.”
“It’s your body, your health, you have to take it seriously,” she said.
Lindsay Peyton is a Houston-based freelance writer.
Lindsay Peyton is ReNew Houston's Transformation columnist.

Folic Acid Powder The champions face many questions. Will Dusty Baker and James Click get new contracts? How about free agents like Justin Verlander?